No matter where you’re located, your best first step in working with Aetna International is to use our secure online provider portal. It’ll help you reduce the amount of time you spend on administrative tasks and give you access to the information you need — whenever you need it.
Use the portal to:
- Verify member eligibility status
- Retrieve Explanation of Benefits (EOB)
- Submit claims and claims reconsiderations, review claim status
- Submit pre-certification or guarantee of payment (GOP) requests
- Update banking/reimbursement details
- Access reference materials
First time users of the portal will need to register. For details on how to register or for log-in assistance, email AetnaInternationalProviderWeb@Aetna.com.
-
![Aetna International (Americas) ID card sample, showing plan details and member names.]()
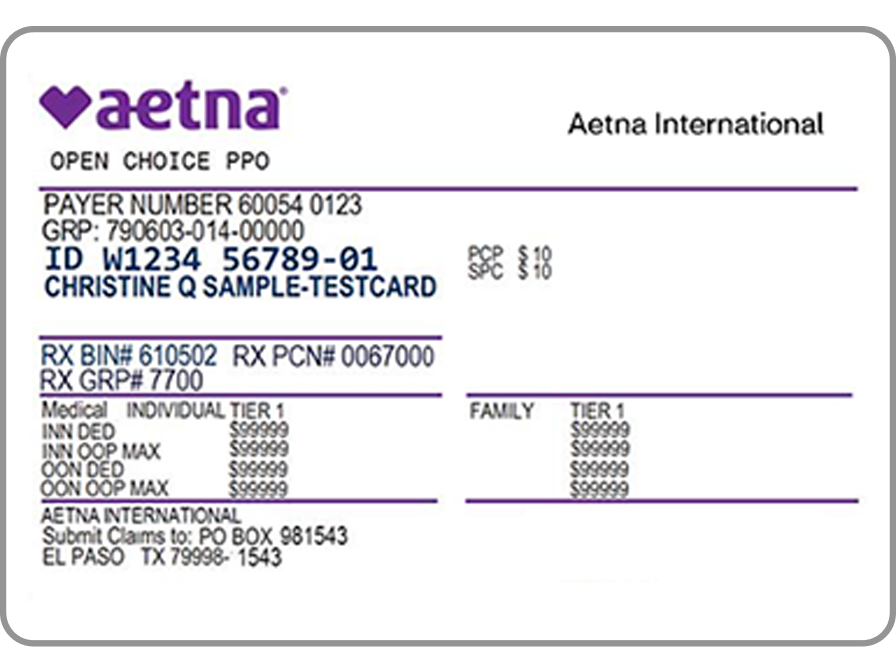
How to identify an Aetna International member
The Aetna International member ID card
Patients that are eligible for direct settlement services will have “Aetna International” at the top of their member ID card, like the card shown here. Refer to the back of the ID card to confirm the correct contact information.
Aetna International members have a Member ID number that normally begins with a “W”.
A member ID card that only has “Aetna” at the top are for plans that provide coverage in the United States only. You can care for these members but they will need to pay for your services and then submit a request to Aetna for reimbursement.
Provider service centers information
Claim submissions
Claims take 30 days on average to process. To ensure timely and accurate claims payment, please review the invoice requirements and submission guidelines.
The best way to submit claims is through the provider portal but you can also email them to CaymanMailboxHGSEscalations@aetna.com using the provider claim form.
The itemized invoice should include:- The total amount of charges, the member’s contribution amount, and the remaining balance to be covered by Aetna International
- Member’s name and member ID number
- Member’s name and date of birth
- Diagnosis (include ICD-10 if available)
- Complete description of all services, date of services, and detailed charges for each service
- Full name and address of provider
Claim status inquiry and reconsiderationThere are several ways to contact us for a claim status update.
For general claims inquiries:- Use the provider portal, or
- Call us at 345-769-3070 (local) or +1-877-851-1661 (toll-free with AT&T USADirect)
- Email InternationalProviderClaimInquiry@Aetna.com (This method is for non-urgent inquiries only. Please allow a minimum of 5 business days for a response.)
For urgent inquiries or questions regarding claim denials:
- Call 345-769-3070 (local) or +1-877-851-1661 (toll-free with AT&T USADirect)
Benefits and eligibilityEligibility status can be verified on the provider portal. Benefit details for members are available by calling 345-769-3070 (local) or +1-877-851-1661 (toll-free with AT&T USADirect) or emailing AIService@Aetna.com.
Pre-certification requestsPre-certification is required for the following services:
- Hospital admissions
- Outpatient surgery
- Lab and X-ray/imaging > $1,000
- Durable medical equipment > $1,000
- Home health services
- Chiropractic services after 6 visits
- Outpatient therapy after 6 visits
- OB ultrasounds after 3 scans
Services may be subject to a penalty of 50% for not complying with these terms.
Submit pre-certification requests on the provider portal or by emailing InternationalProviderServices@Aetna.com. For urgent assistance, call us at 345-769-3070 (local) or +1-877-851-1661 (toll-free with AT&T USADirect).
Note: There are different requirements and exceptions for the Maples and Calder account. Please refer to the Maples and Calder Provider information below.
Provider relations contact information
If you have any questions that you’re unable to answer using this guide or the provider portal, reach out to your Aetna International network manager or email AINetworkManagement@aetna.com.
Local support contact informationStrategic Risk Solutions (Cayman) Limited is available for local support and can assist in answering your questions.
Strategic Risk Solutions (Cayman) Limited
Caribbean Plaza, 2nd Floor, North Building 878 West Bay Road
P.O. Box 1159
Grand Cayman KY1-1102, Cayman Islands
Website: StrategicRisks.com Phone: 345-623-8621
Strategic Risk Solutions shouldn’t be used for claim submissions. Submit claims directly to Aetna International using the information above. -
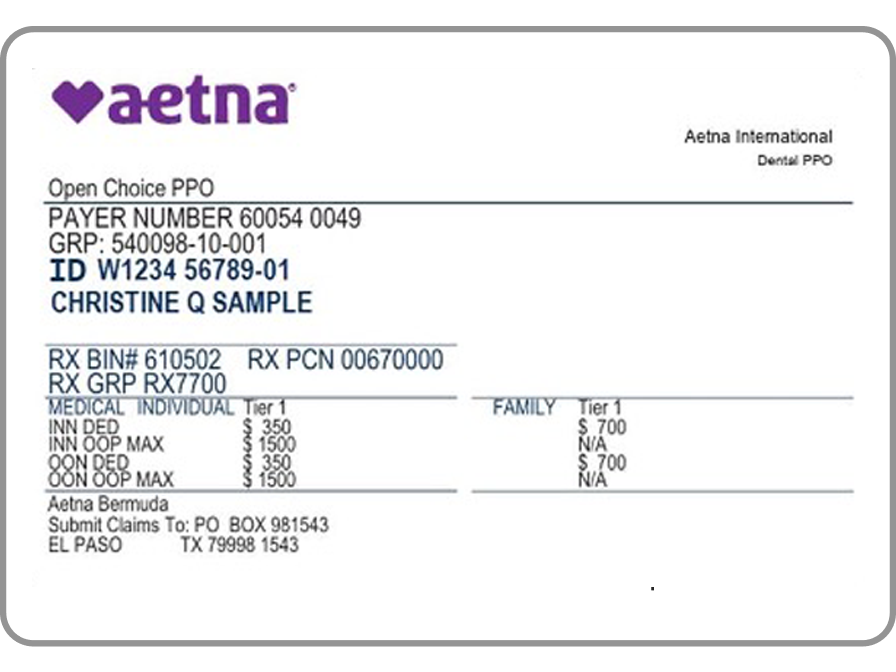
How to identify an Aetna International member
The Aetna International member ID card
Maples and Calder members that are eligible for direct settlement services will have “Aetna International” at the top of their member ID card, like the card shown here. Aetna International members have a Member ID number that normally begins with a “W”.
A member ID card that only has “Aetna” at the top are for plans that provide coverage in the United States only. You can care for these members but they will need to pay for your services and then submit a request to Aetna for reimbursement.Provider service centers information
Claim submissions
Claims take 30 days on average to process. To ensure timely and accurate claims payment, please review the invoice requirements and submission guidelines.
The best way to submit claims is through the provider portal but you can also email them to CaymanMailboxHGSEscalations@aetna.com using the provider claim form.
The itemized invoice should include:- The total amount of charges, the member’s contribution amount, and the remaining balance to be covered by Aetna International
- Member’s name and member ID number
- Member’s name and date of birth
- Diagnosis (include ICD-10 if available)
- Complete description of all services, date of services, and detailed charges for each service
- Full name and address of provider
Claim status inquiry and reconsiderationThere are several ways to contact us for a claim status update.
For general claims inquiries:- Use the provider portal, or
- Call us at +1-855-829-9491 (toll-free with AT&T USADirect)
- Email InternationalProviderClaimInquiry@Aetna.com (This method is for non-urgent inquiries only. Please allow a minimum of 5 business days for a response.)
For urgent inquiries or questions regarding claim denials:
- Call +1-855-829-9491 (toll-free with AT&T USADirect)
Benefits and eligibilityEligibility status can be verified on the provider portal. Benefit details for members are available by calling +1-855-829-9491 (toll-free with AT&T USADirect) or emailing AIService@Aetna.com.
Pre-certification requestsPre-certification is required for the following services:
- Outpatient physical therapy after 6 visits
- Occupational therapy after 6 visits
Services may be subject to a penalty of 50% for not complying with these terms.
Submit pre-certification requests on the provider portal or by emailing InternationalProviderServices@Aetna.com. For urgent assistance, call us at +1-855-829-9491 (toll-free with AT&T USADirect).
Provider relations contact information
If you have any questions that you’re unable to answer using this guide or the provider portal, reach out to your Aetna International network manager or email AINetworkManagement@aetna.com.
-
![Aetna International (Americas) ID card sample, showing plan details and member names.]()
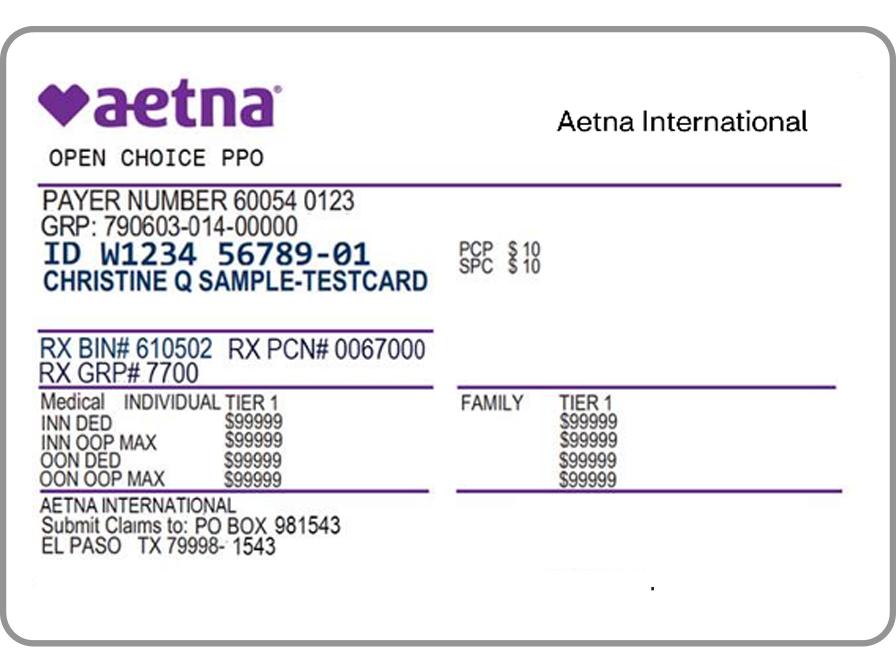
How to identify an Aetna International member
The Aetna International member ID card
Patients that are eligible for direct settlement services will have “Aetna International” at the top of their member ID card, like the card shown here. Refer to the back of the ID card to confirm the correct contact information.
Aetna International members have a Member ID number that normally begins with a “W”.
A member ID card that only has “Aetna” at the top are for plans that provide coverage in the United States only. You can care for these members but they will need to pay for your services and then submit a request to Aetna for reimbursement.
En español: Guía para proveedores de América Latina y el Caribe
Provider service centers information
Claim submissions
Claims take 30 days on average to process. To ensure timely and accurate claims payment, please review the invoice requirements and submission guidelines.
The best way to submit claims is through the provider portal but you can also email them to InternationalProviderClaims@aetna.com using the provider claim form.
The itemized invoice should include:- The total amount of charges, the member’s contribution amount, and the remaining balance to be covered by Aetna International
- Member’s name and member ID number
- Member’s name and date of birth
- Diagnosis (include ICD-10 if available)
- Complete description of all services, date of services, and detailed charges for each service
- Full name and address of provider
Claim status inquiry and reconsiderationThere are several ways to contact us for a claim status update.
For general claims inquiries:- Use the provider portal, or
- Call us at +1-813-775-0190 (direct) or +1-800-231-7729 (toll-free with AT&T USADirect), or
- Email InternationalProviderClaimInquiry@Aetna.com (This method is for non-urgent inquiries only. Please allow a minimum of 5 business days for a response.)
For urgent inquiries or questions regarding claim denials:
- Call +1-800-231-7729 (toll-free with AT&T USADirect).
Benefits and eligibilityEligibility status can be verified on the provider portal. Benefit details for members are available by calling +1-813-775-0190 (direct) or +1-800-231-7729 (toll-free with AT&T USADirect) or emailing AIService@Aetna.com.
Guarantee of payment (GOP)There are several ways to request a GOP from us.
- Use the provider portal, or
- Email InternationalProviderServices@aetna.com (This method is for non-urgent inquiries only. Please allow a minimum of 5 business days for a response.)
For urgent assistance with a GOP:
- Call us at +1-813-775-0190 (direct) or +1-800-231-7729 (toll-free with AT&T USADirect)
Provider relations contact information
If you have any questions that you’re unable to answer using this guide or the provider portal, reach out to your Aetna International network manager or email AINetworkManagement@aetna.com.
We’re here to help!
Questions about joining our network or doing business with us? We can help you get the answers you need.